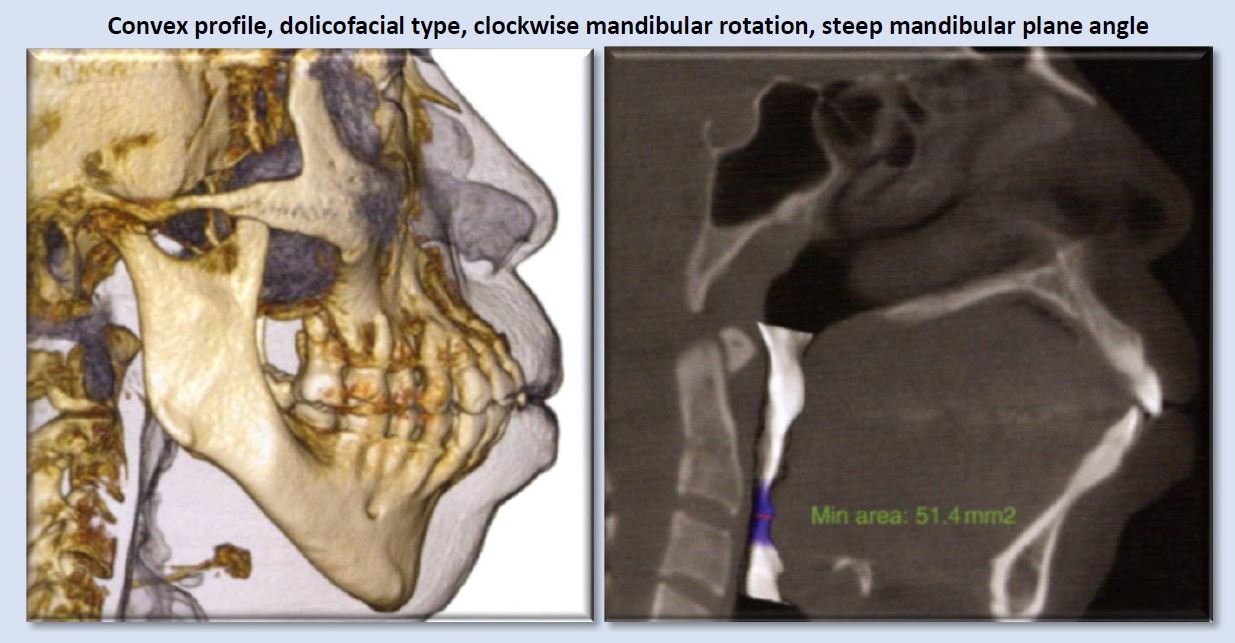
Patient information regarding the presence of sleep disordered breathing (apnea), begins with thorough clinical evaluation. The patient/parent should be interviewed regarding snoring, mouth breathing, medications, and visits to the ENT. An important initial area of assessment includes facial profile (as Class II dolicofacial profiles tend to have more airway problems than other facial types). Resting lip posture, droopy eyes, and the presence of “shiners” (vascular congestion manifested as darkness under the eyes) should be noted. Intraoral findings, such as high palatal vault, narrowed transverse dimensions of the maxillary and/or mandibular dentition, anterior or posterior crossbites with associated functional shifts can be related to airway irregularities.
Once the above questions and clinical assessment are performed, and the findings suggest presence of breathing disorder, imaging is useful to identify possible anatomic and morphologic structures that contribute to risk for presence or development of obstructive sleep-disordered breathing. While sleep apnea is not diagnosed with imaging, cone beam computed tomography (CBCT) exams are valuable in providing three-dimensional or multiplanar views that enable clear definition of irregularities that may be creating obstruction or resistance to airflow through the nasal passages, the nasopharynx, the oropharynx, and the hypopharynx. Some of these irregularities include soft-tissue enlargements or aberrant morphology, bony structures, dental findings, cephalometric measurements, and pathology. Examples in these categories are depicted in images below.
Commonly seen irregularities that indicate risk for presence or development of obstructive sleep-disordered breathing
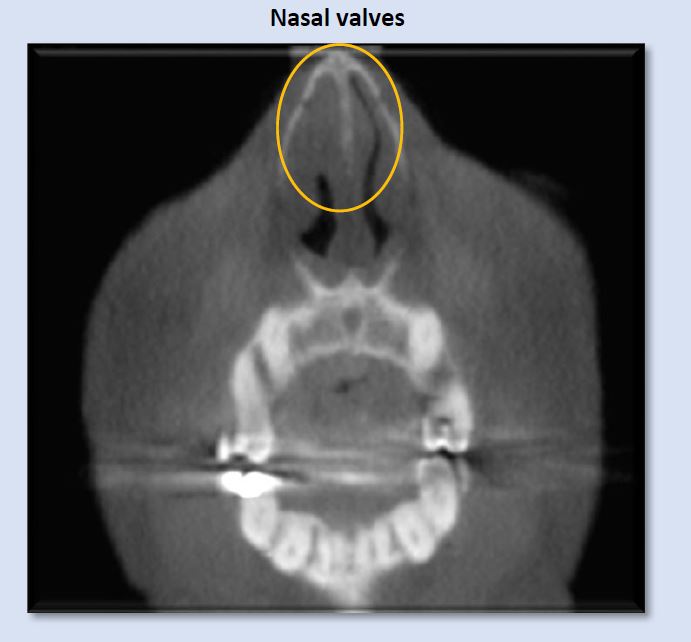
Airflow into the patient’s airway begins at the external, then the internal, nasal valves. These entrances are composed of cartilage, muscle, ligaments, and mucosal soft-tissue, all of which can display irregularities of various etiologies, creating narrowing or blockages. The image above depicts narrowed left internal nasal valve, and constricted right internal nasal valve.
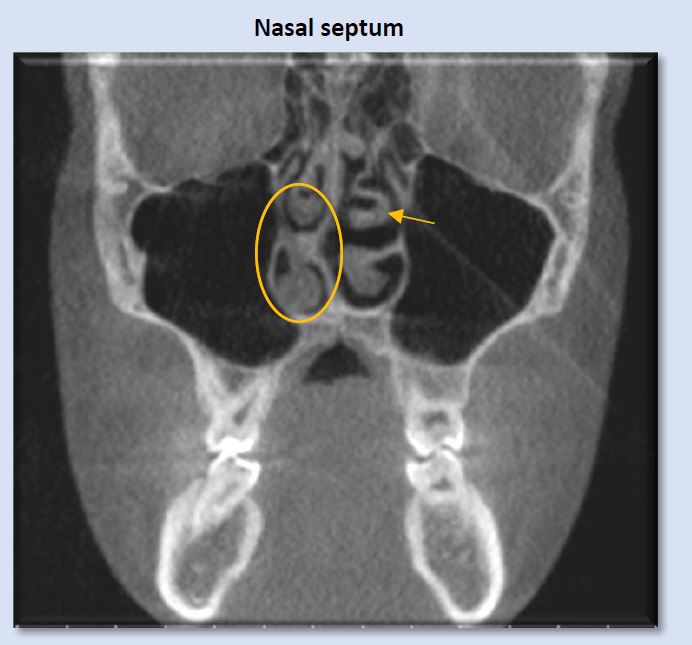
Deviation of the nasal septum is a frequent finding. A large range of variability is seen. Some examples include minor deviation of the full septum, deviation of a small segment, enlarged septal tubercle, formation of a septal spur, and S-shaped contour that deviates both to the right and the left at different levels of the septum. The image above shows right deviation near the level of the right middle meatus, with a bulbous morphology of the septal tubercle contacting the right inferior concha. This can introduce alteration to airflow pattern through the nasal passage.
Note: an anatomic variant of paradoxical turbinate (arrow) is present at the left middle concha. This finding is often without clinical significance, but can create a blockage of the ipsilateral ostiomeatal complex. In this case, the left ostiomeatal complex is patent.
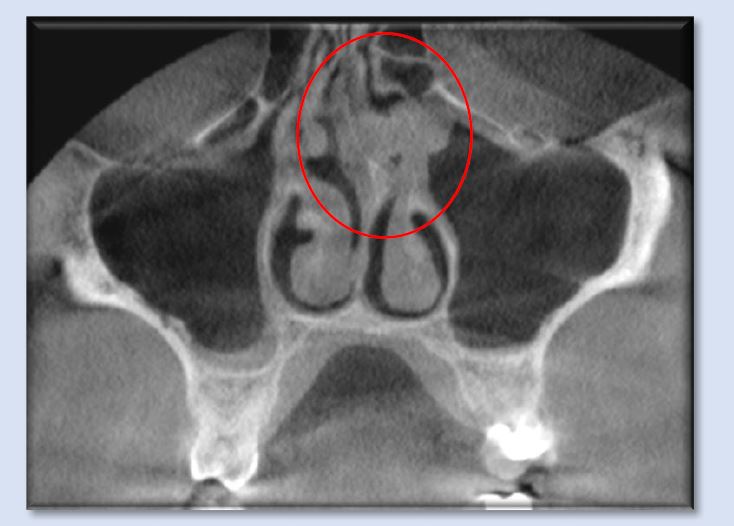
The above image shows septal tubercle/spur formation to the left, where it contacts the superior portion of the left inferior concha and the left middle concha. More superiorly, the nasal septum displays a gradual curvature toward the right. Accompanying these deviations is mild soft-tissue enlargement of the nasal septum as well as mucosal thickening in the superior portion of the left maxillary sinus. The combination of these features is forming obstruction to airflow through the nasal cavity and creating obstruction of the left ostiomeatal complex.
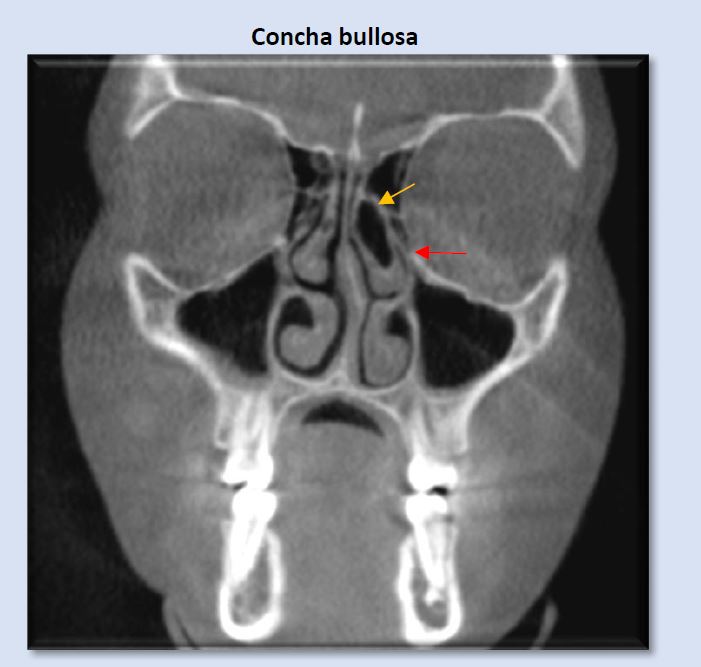
Concha bullosa is an air cell which is most commonly seen occupying the middle concha, either unilaterally or bilaterally. On occasion, smaller conchae bullosa are seen at the superior conchae. They are frequently clinically insignificant, but can influence deviation of the nasal septum and create narrowing or blockage of the ostiomeatal unit. The image above shows an obstructed left ostiomeatal complex (red arrow).
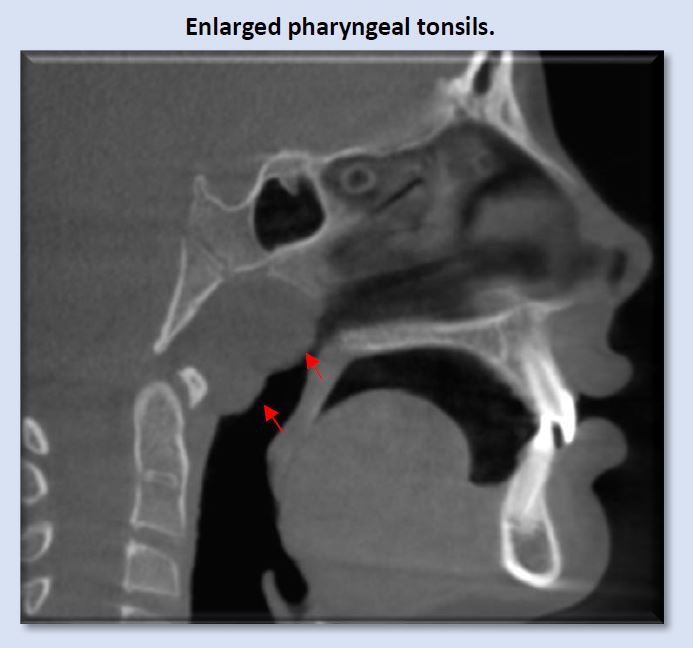
Enlargement of the pharyngeal tonsils (adenoids) is commonly seen, most often in children, which would be expected. If enlargement is seen in adults, more questions regarding etiology are raised, as these tissues typically begin gradual regression after the age of 12. This size enlargement creates significant blockage in the nasopharynx. Note parted lips, even though the condition of deep anterior vertical overlap is present.
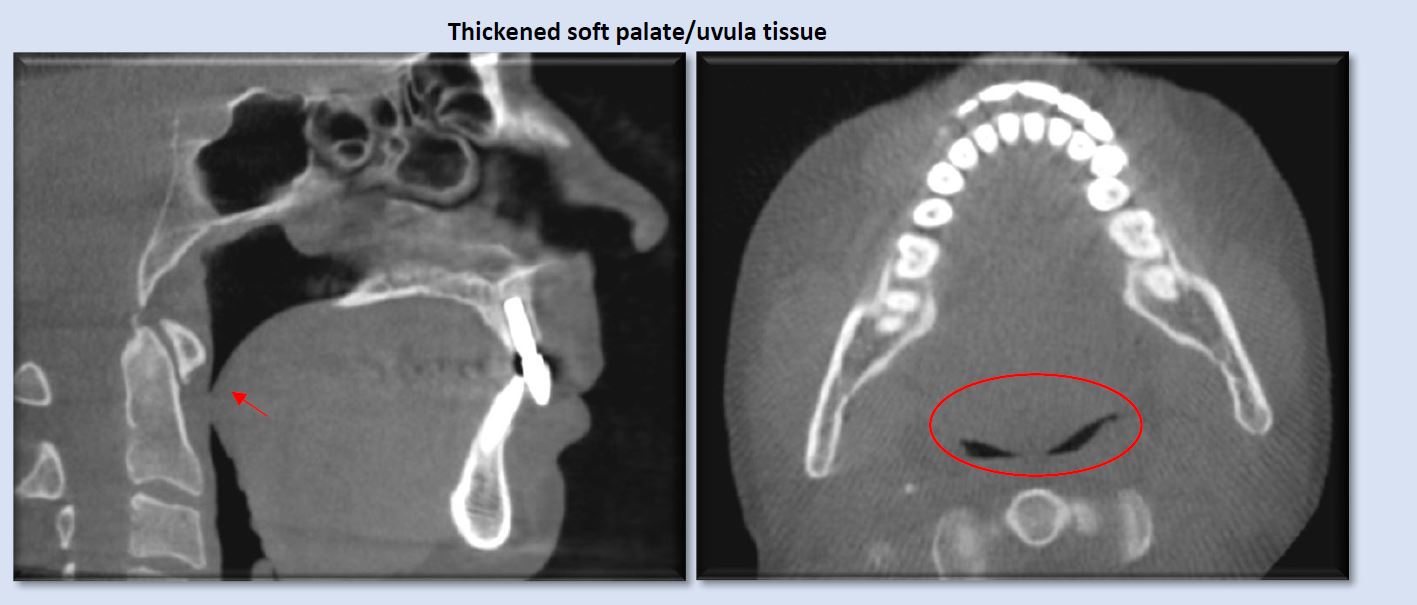
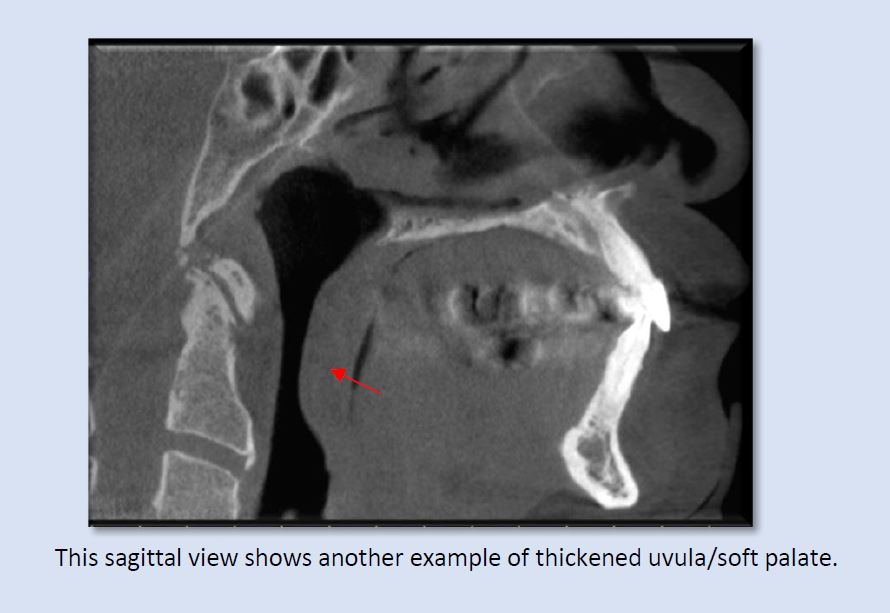
Thickened soft palate and uvula soft-tissue can narrow, and at times, constrict the airway, even while the patient is in an upright position. The presence of obstructive sleep-disordered breathing would be suspected with these patients in supine position. Both sagittal and axial views show the significant narrowing that can be created by swollen or enlarged uvula/soft palate.
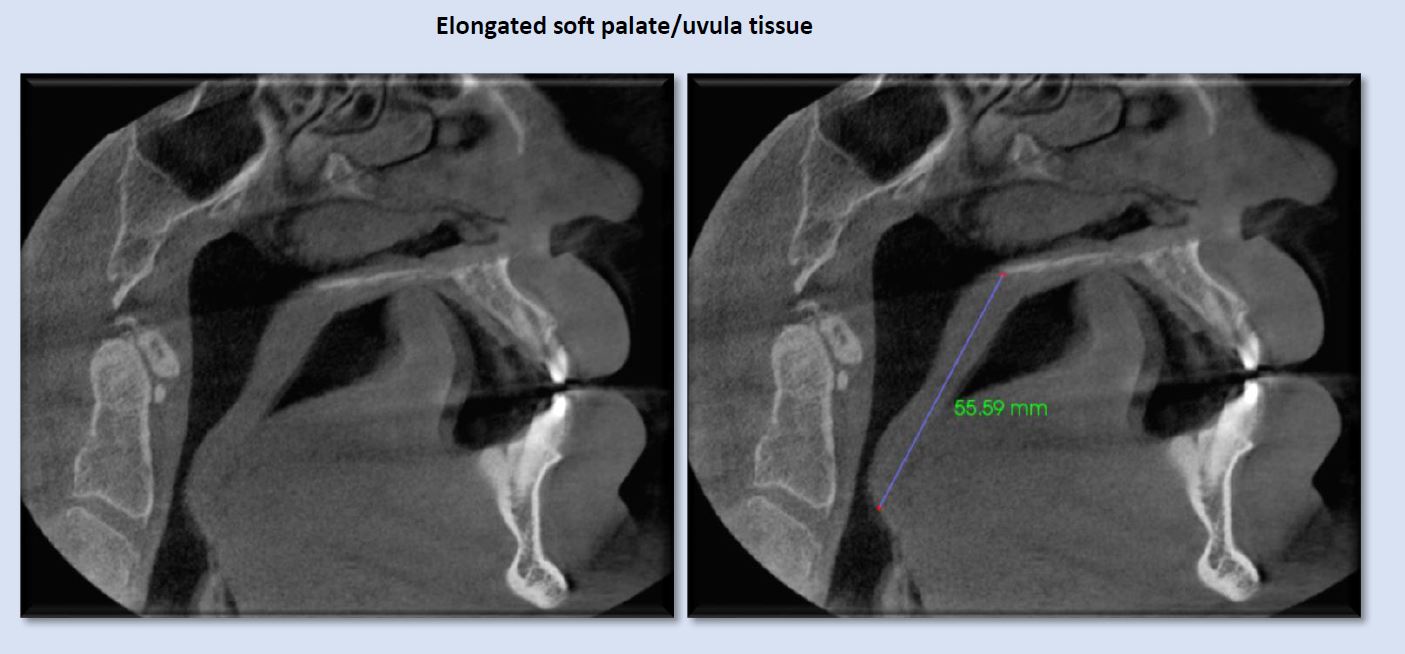
Elongated uvula/soft palate is sometimes implicated in creating narrowing in the oropharynx. Typical length of this soft-tissue complex is approximately 40 mm or less. The image above shows a length that approaches the superior aspect of the epiglottis, with associated airway narrowing.
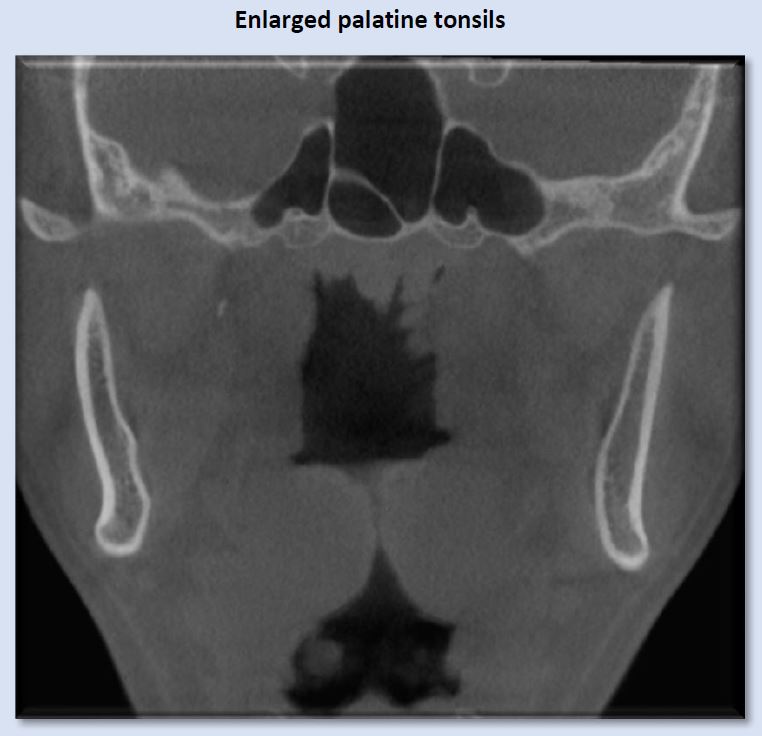
Enlarged palatine tonsils are most commonly seen in children, and demonstrate significant variety in size. The above image depicts considerable enlargement of the palatine tonsils, which is creating blockage of the airway. Regression of the palatine tonsils occurs gradually after the age of 12.
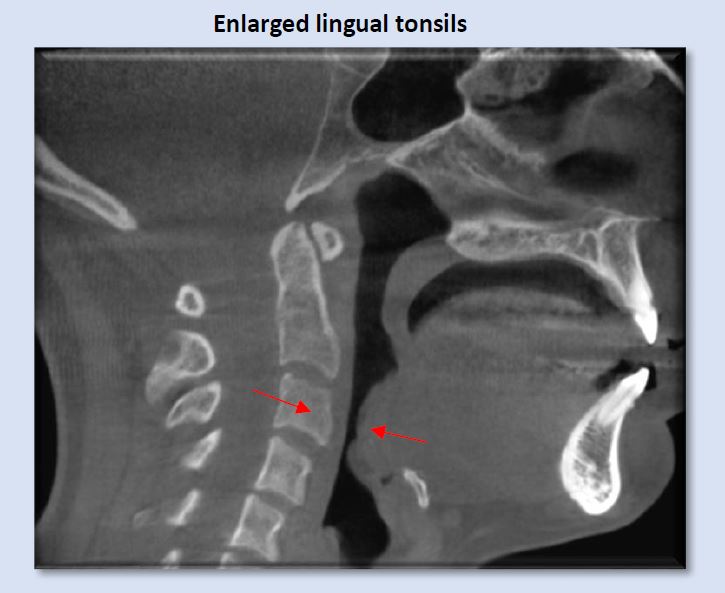
Enlargement of the lingual tonsils is less frequently seen than the pharyngeal or palatine tonsils, but is nevertheless a common finding, and can create significant narrowing of the inferior oropharynx, as shown above. Lordotic curvature of the cervical spine in this instance it exacerbating the constriction.
Commonly seen, but less scrutinized findings relative to risk of sleep-disordered breathing
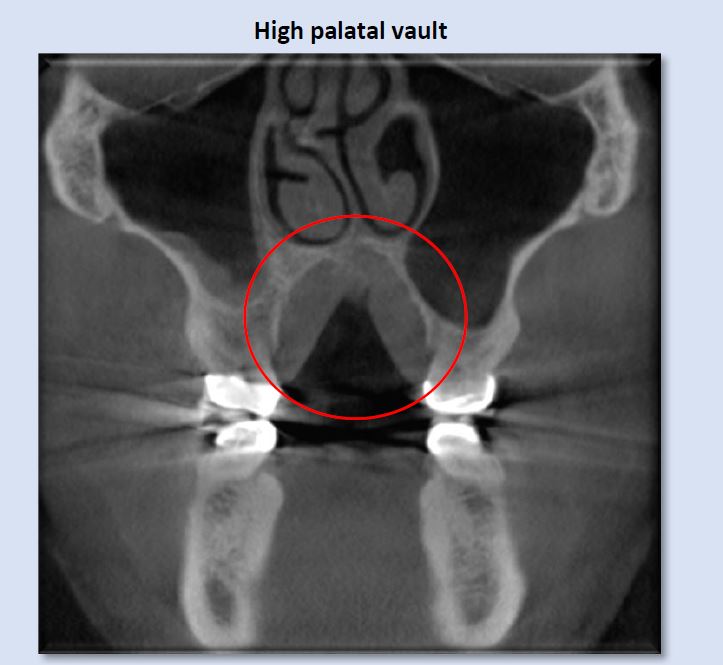
High palatal vault is suggestive of narrowed maxillary alveolar and dental arches, which can result in unilateral or bilateral posterior crossbites, functional shifts, and restriction in the freedom of anterior mandibular movement. It also creates a space for the tongue to be positioned superiorly, which can lead to airway restriction at the superior oropharynx.
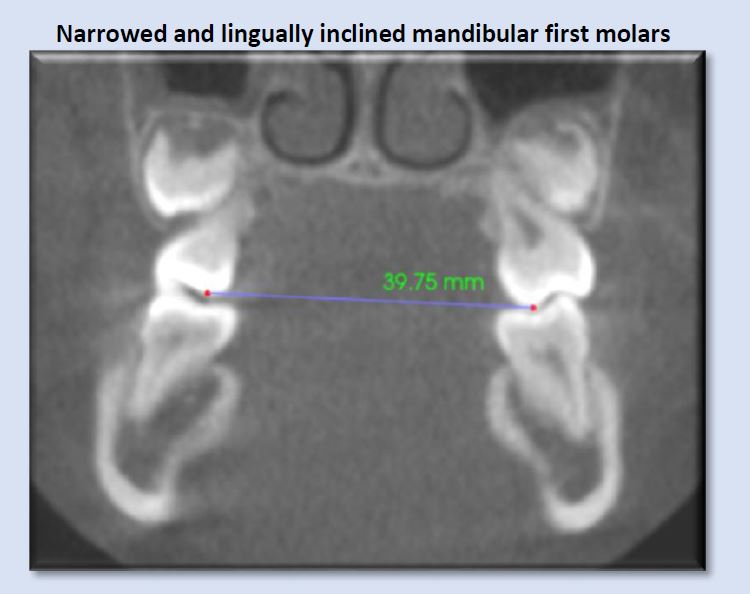
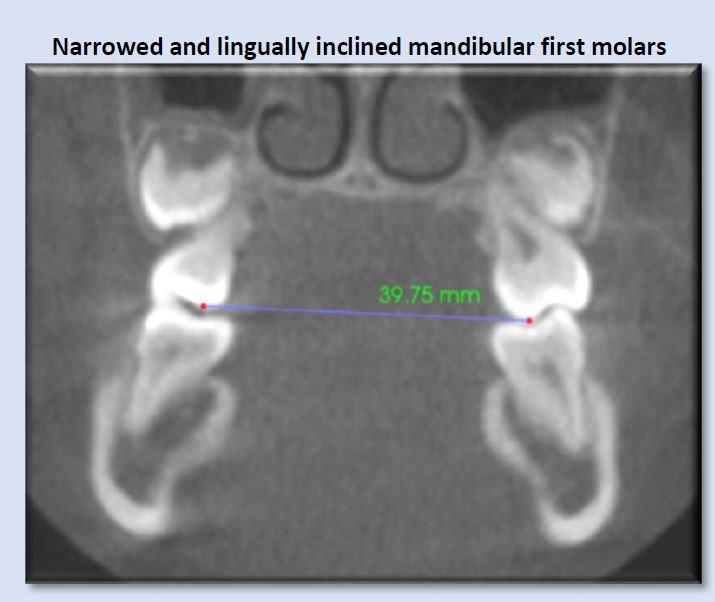
Narrow dental arches often reduce the amount of available tongue space, and may transversely constrict the tongue. This can lead to aberrant tongue shape and position, and subsequent alteration of normal airway space. Rule of thumb: less than approximately 44mm may indicate risk for development of breathing disorder. (Dr. Sean Carlson)
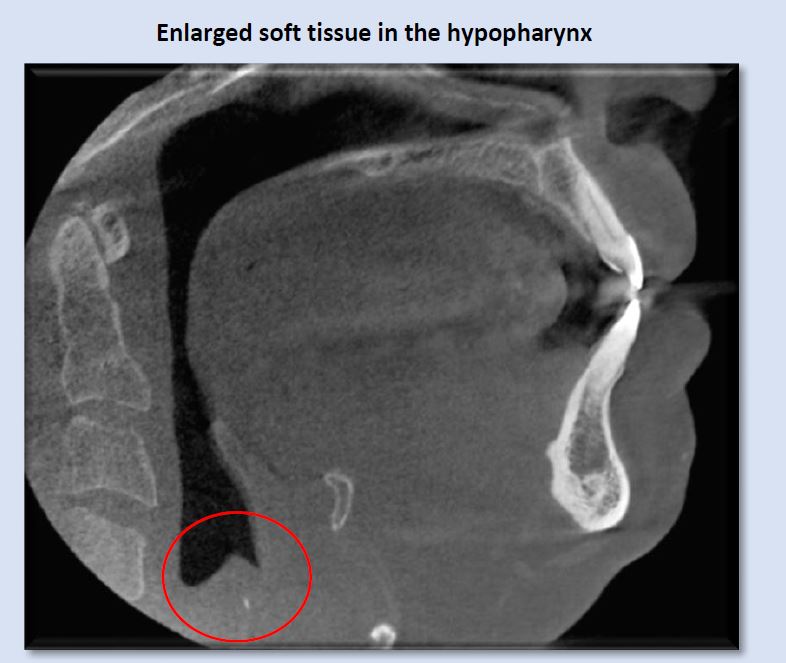
An unusual finding of enlarged soft tissue in the hypopharynx, at the level of the larynx, warrants evaluation medical ENT. The small hyperdensity is likely calcification of arytenoid cartilage.
Narrowed airway dimensions are seen more frequently in cases of this facial growth type than other growth patterns.
Less-commonly seen irregularities that indicate risk for presence or development of obstructive sleep-disordered breathing
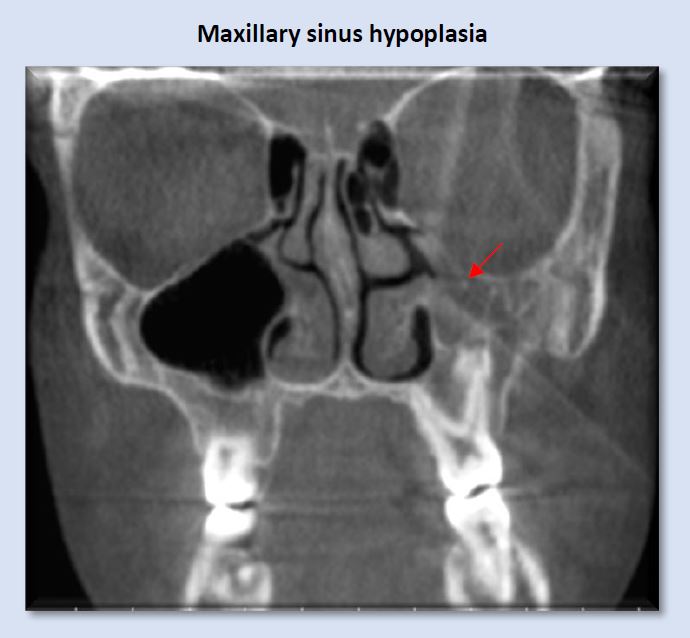
The left maxillary sinus in the image above is considerably smaller than the right, and its lumen is opacified with mucosal thickening. This finding does not necessarily create a condition of sleep-disordered breathing, but should raise suspicion and indicates the need for further assessment.
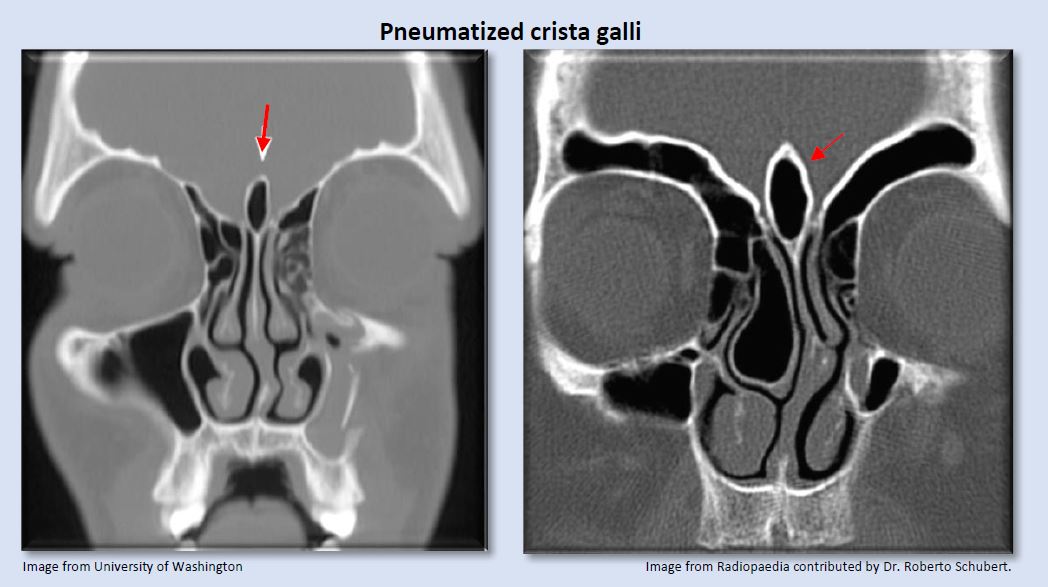
Image from University of Washington Image from Radiopaedia contributed by Dr. Roberto Schubert.
Pneumatized crista galli may communicate with the frontal recess and can potentially obstruct the frontal sinus ostium.
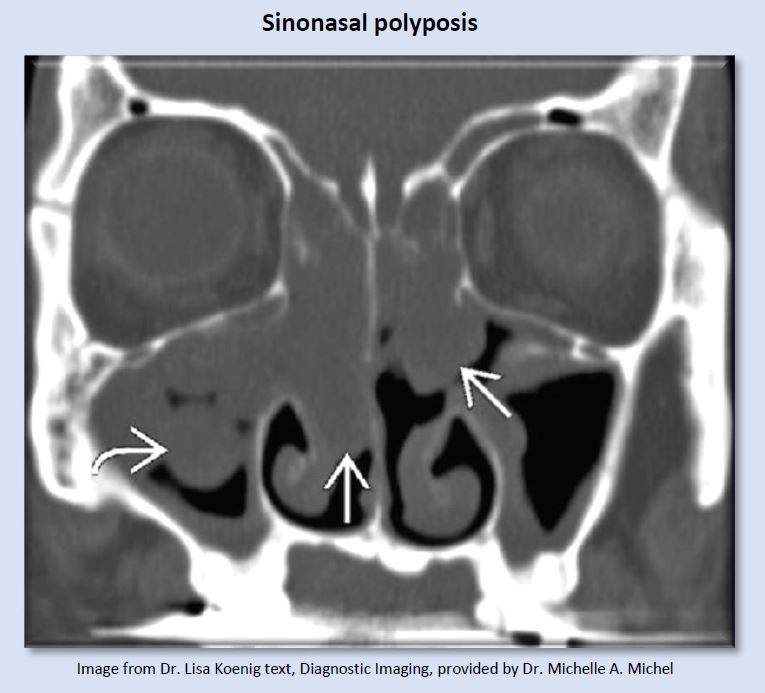
These tissue enlargements are non-neoplastic, inflammatory swellings of sinonasal mucosa that buckles to form “polyps”. Considerable resistance to airflow is created by lesions this size.
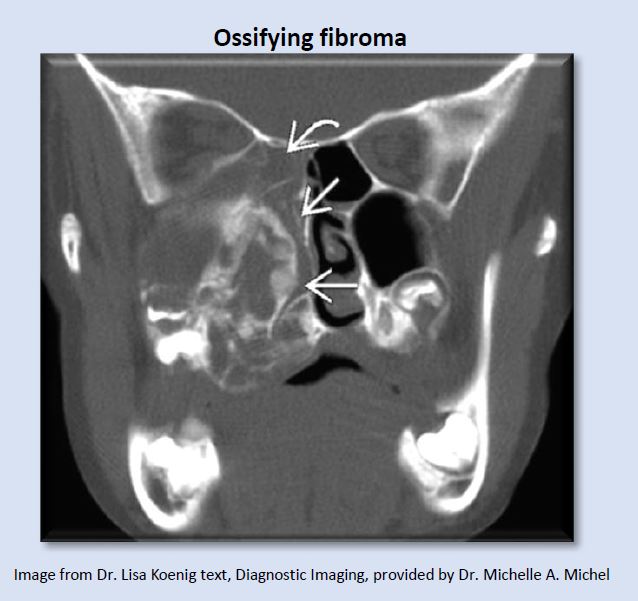
Ossifying fibroma is an expansile benign fibro-osseous neoplasm which can create significant airway blockage.
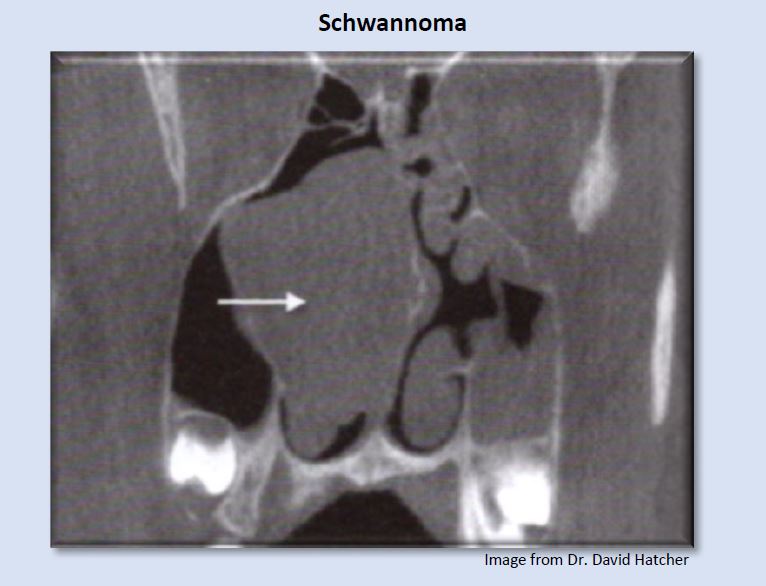
A schwannoma is a normally benign, neural sheet tumor, in this case creating blockage in the right nasal cavity.
The preceding images represent some findings identified on CBCT exams that suggest the possibility of presence or future development of obstructive sleep-disordered breathing. Numerous additional abnormalities not included in this article can create obstructions or disruptions of normal airflow. This flow of air from the environment into the lungs must negotiate a course from the external nasal valves, through the nasal fossa, the nasopharynx, oropharynx, and hypopharynx. Airflow dynamics through this pathway are subject to laws of Poiseuille and Ohm, which show resistance to airflow can create increases in the pressure gradient between the mouth/nose and the alveoli (Hatcher, 2010). Anatomical structures along this pathway involve cartilage, bone, muscles, and mucosa, which are dynamic and can change in dimension and shape in response to normal physiological (swelling and shrinkage of nasal conchae), allergies, infection, and abnormal tissue proliferation, such as polyps or neoplasm.
Click here to submit your scan for an airway assessment